General Medicine - Prefinal examination
MARCH 31,2022
This is an online e log book to discuss our patient identified health data shared after taking his/her guardian signed informed consent. Here we discuss our individual patient problems through a series of inputs from available global online community of experts with a aim to solve those patients clinical problem with collective current best evidence based inputs.This blog also reflects my patient centered online learning portfolio and valuable inputs on the comments box is welcome.
I have been given this case to solve in an attempts to understand the topic of patient clinical data analysis, to develop my competency in reading and comprehending clinical data including history, clinical finding, investigations and come up with diagnosis and treatment.
K.TEJA SREE , ROLL NO:54 , 9th SEM
CASE
A 41 year old male, painter by occupation ,resident of choutuppal came to the hospital with complaints of Itching and scaling of skin all over the body since 3 months
HOPI :
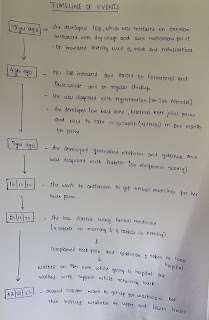
Timeline events:
It gets aggravated in winter and rainy season
He consulted various dermatologists and was given medication but it did not reduce.So he tried different medications and ayurveda.
2011
He went to RMP and injection(dexamethasone and triamcinalone) was given and his condition was relieved for 6months so he got married and after 3- 4 months of his marriage , once again he developed itching and scaling all over the body.
10 days ago he visited local doctor due to severe itching and scaling.then he referred to our hospital.
not a known case of diabetes, hypertension, CAD
no history of TB. epilepsy, asthma
PERSONAL HISTORY:
Appetite : decreased since 3 months
Diet : vegetarian since the last 10years
Bladder & bowel movements : regular
Sleep :inadequate due to itching
Addictions :chronic alcoholic since 15years.
He drinks 90ml of alcohol everyday for few weeks and then discontinues for a while and then he starts again.
Tobacco chewer for more than 15years.
no allergies
TREATMENT HISTORY:
Methotrexate, propysalic ointment, betamethasone, homeopathy and ayurveda since 10yrs
Inj.dexamethasone and triamcinalone every 2-3months for the last 10years
FAMILY HISTORY:
GENERAL EXAMINATION
- Pallor : present
- Icterus : absent
- Cyanosis : absent
- Clubbing : absent
- Lymphadenopathy : absent
- Edema : absent
Vitals
- Pulse rate : 96bpm
- Bp : 100/70mmhg
- Temperature : afebrile
- Respiratory rate : 24cpm
- SpO2 : 98% at room air
SYSTEMIC EXAMINATION
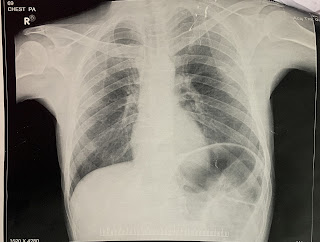
- RESPIRATORY SYSTEM
-position of trachea: central
- normal vesicular breath sounds
-no dyspnea,wheeze
- CARDIOVASCULAR SYSTEM : S1, S2 heard and no thrills and no murmurs
- PER ABDOMEN : soft non tender non distended.
- CNS: higher motor functions are intact.
Clinical pictures
INVESTIGATIONS :
- Random Blood sugar- 102mg/dl -normal
- RFT
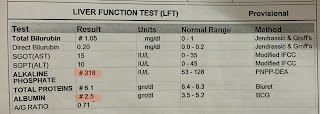
- Liver function test
- Complete urine analysis
- Colour Doppler
- Impression: no evidence of pulmonary, pleural, or cardiac pathology.
- ERYTHRODERMA PSORIASIS
TREATMENT :
- IVF -NS, RL- 75ml/hr with 1amp of optineurin IV OD
- INJ.Thiamine 1amp in 100ml NS IV BD
- liquid paraffin+glycerin+water (apply in equal proportions) three times/day
- tab shelcal OD
- Tab. Dolo 500mg po sos
- Tab. Folic acid 5mg po
- protein x powder with milk
- high protein diet
- tab MVT OD
- tab pregabalin 75mg + tab methylcobalamine 750mcg
- Tab. Lorazepam 2mg po sos
- Fudic cream
- Tab. Escitalopram 5mg OD night
- Tab. Clonazepam 0.5mg
- tab methotrexate 15 mg once weekly for 6 weeks