A 60year old female with AKI with acute liver injury secondary to ?herbal medication with DM,HTN and Bronchial asthma
This is an online E-log book to discuss our patient de-identified health data shared after taking his/ her guardians sign informed consent
Here we discuss our individual patient problems through series of inputs from available Global online community of experts with an aim to solve those patient clinical problem with collective current best evidence based inputs.
This E-log also reflects my patient centered online learning portfolio.
Your valuable inputs on comment box is welcome
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competancy in reading and comprehending clinical data including history, clinical finding, investigations and come up with a diagnosis and treatment plan.
A 60years old female resident of valigonga(bhongir district),a garbage picker by occupation(14years back,use to sale earrings by going door for 7 years,stopped after the death of his son due to snakebite), came to casuality with complaints of weakness of both upperlimbs and lower limbs since 1 day and decreased responsiveness since 1 day.
HISTORY OF PRESENT ILLNESS:
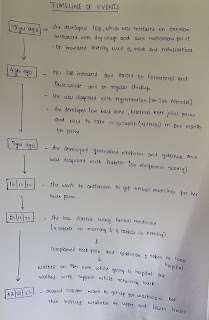
Patient was apparently assymptomatic 15years ago and then developed,shortness of breath,which was increased on exertion and increased in winter seasons and associated with dry cough,and used medications for it (oral medication not known) and on increased severity used oxygen mask and nebulisations after going to local hospital
Later the severity of SOB increased since 4 years and they started inhalations with formeterol and budesonide,and on regular checkup and was diagnosed with hypertension and on Tab.Atenolol 50mg since 4 years and 3 years ago developed generalised weakness and giddiness and went to hospital and was diagnosed to be having diabetes,and on Tab.Metformin 500mg one tab daily.
Patient developed having simultaneous low back ache and bilateral knee joint pains since 4 years and went to hospital and was told to be having ?osteoporotic changes and for the pain used to use pain killers?NSAIDS,with a frequency of 15-20tablets,in one month since 4 years but the pain didnt subsided and as the neighbors suggested the use of herbal medications for her knee pains,and so which last Friday she alone went to anatharam which was 60-70kms away from her home to get herbal medicines,and brought them from there,and she started using them on Wednesday (taken 4 tablets in the morning and 4 tablets in the evening,and at her workplace,and then complained of neckpain and giddiness and then she was taken to local hospital and her Bp was told to be SBP of 150mmHg and as she missed her morning antihypertensive(it was given and fluids were also given.Walked on her own while going to hospital and walked with support while returning back)and at around 1:00am on Thursday,want to get up for washroom,but then noticed the weakness of upperlimbs and lowerlimbs,lowerlimbs>upperlimbs,and she passed urine in the bed as she was unable to walk,and then was taken to valigonda and was referred here for management.
5 episodes of loosestools since yesterday,frst episode was yellowish in colour and remaining four episodes black in colour and watery in consistency.
No episodes of vomitings,fever,headache.
HISTORY OF PAST ILLNESS:
K/c/o HTN since 4years(on T.Atenolol 50mg)
K/c/o DM since 3years( on metformin po/od)
K/c/o Asthma since 4years( on neb. Formatoral and Budesonide)
N/k/c/o TB, epilepsy, CAD, CVD
PERSONAL HISTORY:
Married
Appetite : Normal
Diet : Mixed
(Dietary History : patient wakes up around 6am and goes for 1km walk and then she takes 1glass of milk and 1 roti.
Around 11-11:30 am she eats rice with curry/dal and then again around 2pm she eats rice with curry.
At 4-5pm she takes 1glass of milk or tea
At night she eats rice with curry or 2 rotis)
Sleep : Adequate
At the time of admission (6:30pm)
GCS E3V3M3,
Temp-104.4F
Bp 150/90mmHg
PR 90bpm
RR- 39cpm
Grbs 238mg/dL
Gcs at 4:00am,
Patient is oriented,to place and person,obeying commands
Bp 120/70mmHg
PR 80bpm
Central Nervous System :
Level of consciousness-stuporous
Slurred speech
No Signs of meningeal irritation
Cranial nerves :
1) olfactory nerve : percieves smell on both sides
2) optic nerve : normal visual acuity
3) occulomotor nerve : normal
4) trochlear nerve : normal
6) abducens nerve :normal
(3,4,6 cranial nerves) ; ptosis,squint, nystagmus - absent.
* Ocular movements- present in upward,downward,temporal,nasal gaze
* Pupil- size- normal,shape- central
* Visual reflexes- direct, indirect- reacting to light
5) Trigeminal nerve ; cutaneous sensibility over skin and mucous membranes - present
✓ corneal reflex- present on both sides
✓ deviation of jaw on opening mouth- absent
7) facial nerve; normal
8) vestibuli cochlear nerve; normal
9) glossopharyngeal nerve; Taste sensation on posterior 1/3rd of tongue - present on both sides
✓palatal reflex- present on both sides
10)vagus nerve ; no history of regurgitation of fluids through nose
Palatal reflex- present
11) spinal accessory nerve ; normal
12) hypoglossal nerve ; normal
Motor system
Gait couldn’t be elicited
Power U/L L/L
Right 3/5 3/5
Left 4/5 3/5
Tone U/L L/L
Right Normal Normal
Left Normal Normal
Reflexes
Left biceps and triceps ++
Left Supinator -
Right Supinator -
Right biceps and triceps ++
Lower limbs bilateral knee and ankle absent
Right plantar mute and left plantar extensor
Pupil : reacting to light Pupil- size- normal,shape- central
Cardiovascular System : S1, S2 heard, no murmurs
Respiratory System : Bilateral air entry present.Normal vesicular breath sounds heard.Position of trachea central.
Per abdomen : soft, non tender. No organomegaly.
INVESTIGATIONS:
MRI Brain:
Xray C Spine:on 23/12/2022
- SOAP NOTES:
Bp 160/90mmHg
PR 78bpm
RR- 28cpm
Grbs 193mg/dL
Spo2-98%@RA
- THESIS CASE: