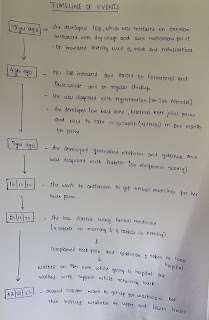
A 30 yr old female with acute gastritis with giddiness
February 2,2023
This is an online E-log book to discuss our patient de-identified health data shared after taking his/ her guardians sign informed consent
Here we discuss our individual patient problems through series of inputs from available Global online community of experts with an aim to solve those patient clinical problem with collective current best evidence based inputs.
This E-log also reflects my patient centered online learning portfolio.
Your valuable inputs on comment box is welcome
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competancy in reading and comprehending clinical data including history, clinical finding, investigations and come up with a diagnosis and treatment plan.
Cardiovascular System : S1, S2 heard, no murmurs
Respiratory System : Bilateral air entry present.Normal vesicular breath sounds heard.Position of trachea central.
Per abdomen : soft, non tender. No organomegaly.
Central Nervous System : Conscious; Speech normal ;
Gait is normal.
MOTOR SYSTEM
Tone RT. LT
UL Hypertonic N
LL. N. N
Power
UL 5/5 5/5
LL. 5/5. 5/5
Reflexes
Biceps-. Exaggerated exaggerated
Triceps-.exaggerated. exaggerated
Supinator-
Exaggerated. Exaggerated
Knee-. Exaggerated. Exaggerated
Ankle-. Exaggerated. Exaggerated
Plantar-.
Babinski+. Flex
Jaw jerk +
*Sensory system*
spino thalamic. Rt. Lt
Crude touch. N. N
Pain. N. N
Temp. N. N
Posterior column
Fine touch. N. N
Vibration. N. N
Position sense.
UL. 10/10. 10/10
LL 5/10. 10/10
Romberg sign- swaying more to right side
Cortical. Rt. Lt
Graphaesthesia-. N. N
Stereognosis- N. N
Cerebellar signs
No dysdiadokokinesia
No finger nose incoordination
No finger finger incoordination
Autonomic nervous system
Postural hypotension:-
Supine - 110/70 mm hg
Standing- 100/ 60 mm hg
Pulse:-
Supine - 80 bpm
Standing- 101 bpm
Signs of meningeal irritation:-
No neck stiffness
Kernig's sign- negative
Brudzinski's sign- negative
INJ.PAN 40mg IV OD
INJ. Zofer 4mg IV TID
Tab. PCM 650mg PO SOS
INJ. NEOMOL 1gm IV SOS(if temp >101F)
INJ. OPTINEURON 1AMP IN 500ml NS IV OD
WATCH FOR HYPOTENSIVE SYMPTOMS
INJ.PAN 40mg IV OD
INJ. Zofer 4mg IV TID
Tab. PCM 650mg PO SOS
INJ. NEOMOL 1gm IV SOS(if temp >101F)
INJ. OPTINEURON 1AMP IN 500ml NS IV OD
WATCH FOR HYPOTENSIVE SYMPTOMS
INJ.PAN 40mg IV OD
INJ. Zofer 4mg IV TID
Tab. PCM 650mg PO SOS
INJ. OPTINEURON 1AMP IN 500ml NS IV OD
INJ. Promethazine 25mg IM/OD
WATCH FOR HYPOTENSIVE SYMPTOMS
INJ.PAN 40mg IV OD
INJ. Zofer 4mg IV TID
Tab. PCM 650mg PO SOS
INJ. OPTINEURON 1AMP IN 500ml NS IV OD
INJ. Promethazine 25mg IM/OD
WATCH FOR HYPOTENSIVE SYMPTOMS