OCTOBER 22
This is an online e log book to discuss our patient identified health data shared after taking his/her guardian signed informed consent. Here we discuss our individual patient problems through a series of inputs from available global online community of experts with a aim to solve those patients clinical problem with collective current best evidence based inputs.This blog also reflects my patient centered online learning portfolio and valuable inputs on the comments box is welcome.I have been given this case to solve in an attempts to understand the topic of patient clinical data analysis, to develop my competency in reading and comprehending clinical data including history, clinical finding, investigation.
K.TEJA SREE , ROLL NO:54 , 9th SEM
CASE
A 28y old male came to the opd with chief complaints of
fever since 10 to 25 days and
SOB since 5 to 6 days.
HOPI:
Patient was apparently asymptomatic 15 days back then developed fever which was incidious in onset and non progressive. It was associated with chills and dry cough. Not associated with cold.
C/O SOB since 5 to 6 days that progressed from grade 2 to grade 3. Not associated with pedel edema and loose stools.
No h/o bleeding manifestations, bleeding gums, malena, hemoptysis, hemetemesis.
PAST HISTORY:
No h/o similar complaints of in the past. No h/o DM, HTN, CAD, Asthma, TB.
PERSONAL HISTORY :
Patient has a mixed diet with decreased appetite and adequate sleep. Patient has constipation. Normal bladder filling and micturition. No addictions.
Appetite: decreased
Diet : mixed
Patient has constipation
Micturition : normal
Sleep :adequate
No addictions
No significant family history.
GENERAL EXAMNATION:
Patient is c/c/c.
No pallor, icterus, cyanosis, clubbing, lymphadenopathy, pedel edema.
VITALS:
temp: 101 F
PR: 98 bpm
RR: 18 cpm.
BP: 90/70 mmhg.
SPO2: 96% at RA.
RESPIRATORY SYSTEM:
position of trachea - central
normal vesicular breath sounds
Abdomen: soft and non-tender.
CVS: S1, S2 heard
no thrills and murmurs.
CNS: No focal deformities.
INVESTIGATIONS:
1) SERUM ELECTROLYTES:
NA: 134.
K: 4.6
CL: 96.
2) Serum Creatinine: 1.1
3) Serum Urea: 32 mg/dl
4) LFT:
TB: 0.94
DB: 0.3
SGOT: 117
SGPT: 114
AP: 183
TP: 5.7
A: 2.3
A/G RATIO:.0.68
5) Serology: negative
6) HEMOGRAM:
Hb: 11.9
TC: 7,700
N/L/E/M/B: 80/16/2/2/0
PLT: 2.2 lakh
7) MP STRIP : Negative.
8) CUE : normal.
9) USG: NORMAL.
10) RAPID DENGUE: Negative.
HEMOGRAM (20/10/21)
22/10/21
SERUM ELECTROLYTES (20/10/21)
LFT (20/10/21)
CUE (20/10/21)
SERUM CREATININE
RAPID DENGUE TEST
SEROLOGY: NEGATIVE
USG abdomen
PROVISIONAL DIAGNOSIS :
VIRAL PYREXIA.
TREATMENT:
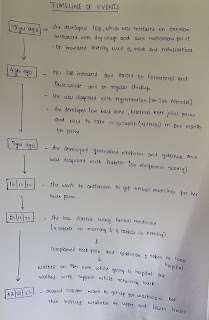
DAY 1
1)IV Fluids NS and RL -100 ml/hr
2)inj optineurin 1 amp in 100 ml/hr IV bd
3)inj Monocef 1gm IV bd
4)Tab.Doxycyline 100 mg po bd
5)inj pan 40 mg IV od BBF
6)inj zofer 4 mg IV SoS
7) inj Neomol 1 gm iv SoS
8)Tab .Dolo 650 mg po sos
9 ) Bp temp,PR monitoring 6 th hourly ,inform SOS
DAY 2
1)IV Fluids NS and RL -100 ml/hr
2)inj optineurin 1 amp in 100 ml/hr IV bd
3)inj Monocef 1gm IV bd
4)Tab.Doxycyline 100 mg po bd
5)inj pan 40 mg IV od BBF
6)inj zofer 4 mg IV SoS
7) inj Neomol 1 gm iv SoS
8)Tab .Dolo 650 mg po sos
9 ) Bp temp,PR monitoring 6 th hourly ,inform SOS
FEVER CHART
23/10/2021- discharged