60 yr old male with SOB since 15 days on and off
October 19,2021
This is an online e log book to discuss our patient identified health data shared after taking his/her guardian signed informed consent. Here we discuss our individual patient problems through a series of inputs from available global online community of experts with a aim to solve those patients clinical problem with collective current best evidence based inputs.This blog also reflects my patient centered online learning portfolio and valuable inputs on the comments box is welcome.I have been given this case to solve in an attempts to understand the topic of patient clinical data analysis, to develop my competency in reading and comprehending clinical data including history, clinical finding, investigation.
K. TEJA SREE , 9th Sem, ROLL NO - 54
case
A 60 yr old male came to the casuality with the chief complaints of SOB since 15 days on and off and pedal edema since 2 months.
HOPI:
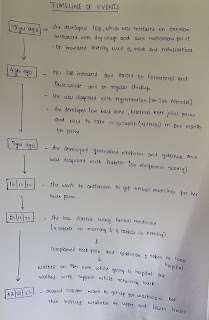
Patient was apparently asymptomatic 2 years back. Then he complaints of small ulcer over left leg and went to hospital ( no history of trauma) and on regular medication for ulcer and also diagnosed with CRF and on regular medication.
Since 2 months patient complaints of pedal edema which is of pitting type and went to local hospital and there he was diagnosed with B/L CRF and baseline creatinine around 4.5.
Since 15 days he is having SOB on & off (grade 4)
It is associated with orthopnea.
It is not associated with chest pain,palpitations, PND, syncopal attacks.
He complaints of decreased urine output ( since yesterday morning i.e, since 17/10/2021 morning)
No history of burning micturation.
PAST HISTORY:
- History of seizures in past
- No history of hypertension, diabetes,TB
PERSONAL HISTORY:
- Diet : veg
- Appetite : reduced
- Sleep : adequate
- Bowel and bladder:Regular
- Addictions : alcohol since 40yrs {Daily 90-180ml/day} Smoking 18-20 beedis/Day
- Allergies : No known food or drug allergies
FAMILY HISTORY:
- insignificant
GENERAL EXAMINATION
Patient is conscious, cooperative and coherent
Well oriented to time, place and person
He is moderately built and moderately nourished.
He was examined after taking consent
- Pallor : present
- Icterus : absent
- Cyanosis : absent
- Clubbing : absent
- Lymphadenopathy : absent
- Edema : B/L pedal edema pitting type
Vitals
- Pulse rate : 96bpm
- Bp : 120/80mmhg
- Temperature : afebrile
- Respiratory rate : 26cpm
- SpO2 : 88% at room air
99% at 6L O2
SYSTEMIC EXAMINATION
- RESPIRATORY SYSTEM
-position of trachea: central
-B/L Crepts are heard on auscultation
- CARDIOVASCULAR SYSTEM : S1, S2 heard and no thrills and no murmurs
- PER ABDOMEN : soft non tender non distended.
- CNS: higher motor functions are intact.
INVESTIGATIONS:
- 18/10/21 chest xray
- Pitting edema
- 18/10/21 ABG
- 18/10/21 BLOOD UREA
- 18/10/21 hemogram
- 18/10/21 CUE
- 18/10/21 LFT
- 18/10/21 Troponin-1
- 18/10/21 HIV 1/2 rapid test
- 18/10/21 Hbs-ag
- Blood group
- 18/10/21 blood sugar random
- ECG
- USG abdomen
- SARS CoV 2
PROVISIONAL DIAGNOSIS
- Chronic renal failure with HFrEF with Uremic encephalopathy
Treatment
- Tab LASIX 40mg BD
- Tab PANTOP 40mg BD
- Fluid restriction less than 1.5L/day
- Salt restriction less than 2g/day
- Tab shelcal OD
- Inj erythropoietin 4000 Weekly once
- Tab orofer BD
- Tab Ecospirin BD
- Tab metxl 25mg OD
- Tab hydralazine 25mg OD
- Neb duolin 4th hourly
- Budecort 6th hourly
Unfortunately he passed away on 24/10/2021 afternoon