June 12,2021
This is online E-blog, to discuss our patient de-identified health data shared after taking her guardian's signed informed consent.
Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve the patients clinical problem with current best evidence based input.
This E-blog also reflects my patient's centred online learning portfolio.
I have been given this case to solve in an attempt to understand the topic of "Patient Clinical Data Analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
K.TEJA SREE, 8th Sem , ROLL NO-54
12/06/2021
CASE
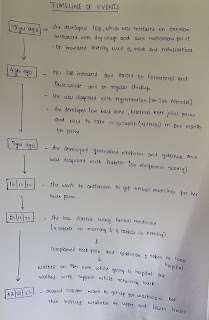
70 Year old male came to the OPD on 15/05/2021 with chief complaints of
Fever since 10 days
Dry cough since 10 days
Shortness of breath since 4 days
HISTORY OF PRESENT ILLNESS
Patient was apparently asymptomatic since 10 days back and then he developed
fever since 10 days which was insidious in onset and not associated with chills and rigors which was subsided on medications.
dry cough since 10 days
shortness of breath since 4 days which was insidious in onset and gradually progressed to Grade-3 according to MMRC grading.
NO history of cold, chest pain, headache, loss of taste and smell
patient was tested positive for (RTPCR)COVID, 10/25 for which he was admitted.
PAST HISTORY
He is not a known case of Hypertension, Diabetes mellitus, Asthma, CAD, TB
No surgeries in the past.
PERSONAL HISTORY
Diet- Mixed
Appetite- normal
Bowel and bladder movements - regular
Sleep - adequate
No allergies
No addictions
FAMILY HISTORY
Insignificant
GENERAL EXAMINATION
The patient is examined with informed consent.
Patient is conscious, coherent and cooperative ,is well oriented to time, place and person.
He is moderately built and nourished
Pallor : absent
Icterus : absent
Cyanosis : absent
Clubbing : absent
Lymphadenopathy : absent
Edema : absent
Dehydration : mild
VITALS:
On the day of admission - 15/05/2021
Temperature :98.7F
Pulse:82 BPM
Respiratory rate : 22 cycles/min
BP : 110/60mm HG
SPO2 : 86% at Room Air
16/05/2021
Temperature : 98.6F
Pulse : 90 BPM
Respiratory rate : 22 cycles/min
BP : 110/60mm HG
SPO2 : 92% at Room Air
17/05/2021
Temperature : 98.6F
Pulse:98 BPM
Respiratory rate : 22 cycles/min
BP : 130/80mm HG
SPO2 : 96% at Room Air
GRBS : 326md/dl
18/05/2021
Temperature :
Pulse:96 BPM
Respiratory rate : 22 cycles/min
BP : 110/80mm HG
SPO2 : 96% at Room Air
GRBS : 164mg/dl
19/05/2021
Temperature : 98.6F
Pulse:94 BPM
Respiratory rate : 22 cycles/min
BP : 120/70mm HG
SPO2 : 95% at Room Air
GRBS : 478mg/dl
20/05/2021
Temperature : 98.7F
Pulse:86 BPM
Respiratory rate : 22 cycles/min
BP : 120/70mm HG
SPO2 : 96% at Room Air
GRBS : 469mg/dl
SYSTEMIC EXAMINATION
CVS:
· S1 and S2 heart sounds heard.
· No murmurs heard.
Respiratory system:
· Bilateral air entry +
Dyspnea : present
vesicular breath sounds
·
CNS:
Intact
oriented to time, place and person
Abdomen
· Soft and non-tender.
· Bowel sounds were heard.
· No organomegaly.
INVESTIGATIONS
16/05/2021RFT : UREA : 80mg/dl
CREATININE : 1.0mg/dl
URIC ACID : 5.7mg/dl
CALCIUM : 9.9mg/dl
PHOSPHORUS : 2.6mg/dl
SODIUM : 136mEq/L
POTASSIUM : 4.0mEq/L
CHLORIDE : 99mEq/L
ABG : PH : 7.42
PCO2 : 32.9
PO2 : 72.5
HCO3 : 21.0
BEB : -2.4
BEecf : -2.7
TCO2 : 43.3
O2 Sat : 91.7
O2 count : 13.5
LFT : Total bilurubin : 0.99mg/dl
Direct bilurubin : 0.18mg/dl
SGOT(AST) : 26IU/L
SGPT (ALT) : 32IU/L
ALKALINE PHOSPHATE : 145IU/L
Total proteins : 6.8gm/dl
ALBUMIN : 2.9gm/dl
A/G Ratio : 0.73
CBP : HAEMOGLOBIN : 13.6gm/dl
TOTAL COUNT : 5000 cells/cu.mm
NEUTROPHILS :83%
LYMPHOCYTES : 11%
EOSINOPHILS : 03%
MONOCYTES : 04%
BASOPHILS : 00%
PLATELET COUNT : 1.75
SMEAR : Normocytic normochromic with relative neutrophilia.
20/05/2021
BLOOD UREA :56mg/dl
SERUM CREATININE : 1mg/dl
CBP : HAEMOGLOBIN :13.4gm/dl
TOTAL COUNT : 7900 cells/cu.mm
NEUTROPHILS :90%
LYMPHOCYTES : 05%
EOSINOPHILS : 02%
MONOCYTES : 02%
BASOPHILS : 00%
PLATELET COUNT : 2.02
SMEAR : Normocytic normochromic with neutrophilia.
ECG :
PROVISIONAL DIAGNOSIS :
VIRAL PNEUMONIA SECONDARY TO COVID-19
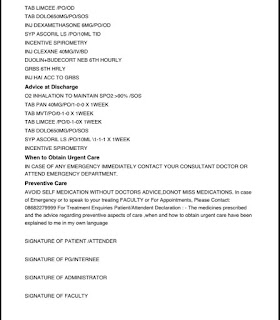
TREATMENT REGIMEN :
On 15/05/2021:
O2 inhalation @NIV to maintain SPO2 >90%
Inj. DEXAMETHASONE6mg/IV/OD
Nebulisation with Duolin,budecort, mucomyst 8th hourly
Syrup. GRILINCTUS
Tab. PANTOP 40md/OD
Tab. LIMCEE OD
Tab. PARACETAMOL 650mg
IVF 20ns with optineuron @75ml/hr
BP, PR, SPO2 monitoring
Temperature charting
Patient discharged on LAMA on 20/05/2021.
I would like to thank Dr.Rakesh biswas sir for giving me this opportunity.